John A. Macoviak, MD, is a Google Scholar and retired heart transplant surgeon based in California. John Macoviak, MD, now focuses on his work as an author of non-fiction and fiction. In this article John A. Macoviak writes about something good from the medical device world after the approval in 1995 by the FDA of publicly available defibrillators, methods and apparatus used for defibrillating a heart, a great lifesaving advance. Internal surgically implanted cardiac defibrillators and more depth on the often-brutal controversies in heart transplantation which have been and will be further addressed in other articles.
Dr. John A. Macoviak writes on range of medical topics like heart transplantation and Washington DC POLITICS which created powerful media attention at the Heart Transplant Consortium of 7 Hospitals. His mentor Dr. Norman E Shumway was a powerful master of publicity in Palo Alto and loomed large in the small world of heart surgeons globally enshrined in history. Shumway put Dr. Macoviak in the media spotlight when a boy from Poland was flown in for complex congenital heart surgery. Shumway assigned Macoviak to address some of his famous successful outcomes and referrals including 30 heart transplant recipents for all walks of life, and others who sought Shumway’s considred opinion including Edward Teller, Jay Pritzker Sr., Milton Friedman.
The young new surgeon was a never before politician, not of billionaire family heritage unlike his peer co-chief resident Bill Frist. By birth Dr. Macoviak grew up in a coal patch town of less than 500 people in Harwood, Pennsylvania. He had strong genes of resiliency for serving others at all costs like his humble devout parents, his father a WWII Master Sergeant who made sure his 65 men came home honorably, safely and heroically. He never wanted to discuss that. His son was always striving to a fault to make an industrious earned positive difference for family, mentors, friends and patients. John A. Macoviak as a newly trained heart transplant surgeon was retained by the most affluent DC paradigms, leaders and systems, pressured and obliged to follow educate-the-public by requests of the media and Consortium caught up in the competitive town-gown syndrome dating centuries past.
By DC politics and 7 hospitals all wanting recognition, Georgetown, Dr. Macoviak’s college Cum Laude and medical school Magna Cum Laude alma mater was precluded from being the sole heart transplant center. Instead the consensus newly default created in 1988 the Seven Hospital Washington Regional Heart Transplant Consortium. In the consortium Macoviak performed the first thirty heart transplants, one compassionate experimental heart pancreas transplant on a diabetic nuclear physicist having normal kidneys with Hans Sollinger MD the world’s leading pancreas transplant surgeon at the University of Wisconsin. All plans of action were approved by the full Ethics Committee and co-surgeons Department Chairs Paul Corso MD (Cardiac Surgery) and Jimmy Light MD (Renal Transplant Surgery).
Dr. Macoviak also performed the first LVADs in the US after Texas Heart at Medstar. Also he performed one heart transplant at GW with Ben Aaron, and one heart transplant at Georgetown with Nevin Katz MD. John A. Macoviak writes often about experiences on faculty at Harvard, Stanford, Mayo, Georgetown and Penn and their world-renowned Professors of Cardiology and Cardiac Surgery. He was fortunately blessed by great mentors who without exception always fully supported Macoviak without reservation publicly and privately in the face of archetypically outwardly-humble but quietly-operating clandestine competitor contrarians, whom his daughters said “they had to – they all wanted to be you” and “because it was a very challenging exhausting against all odds nonetheless successful important legacy, built standing on the shoulders of great mentors.”
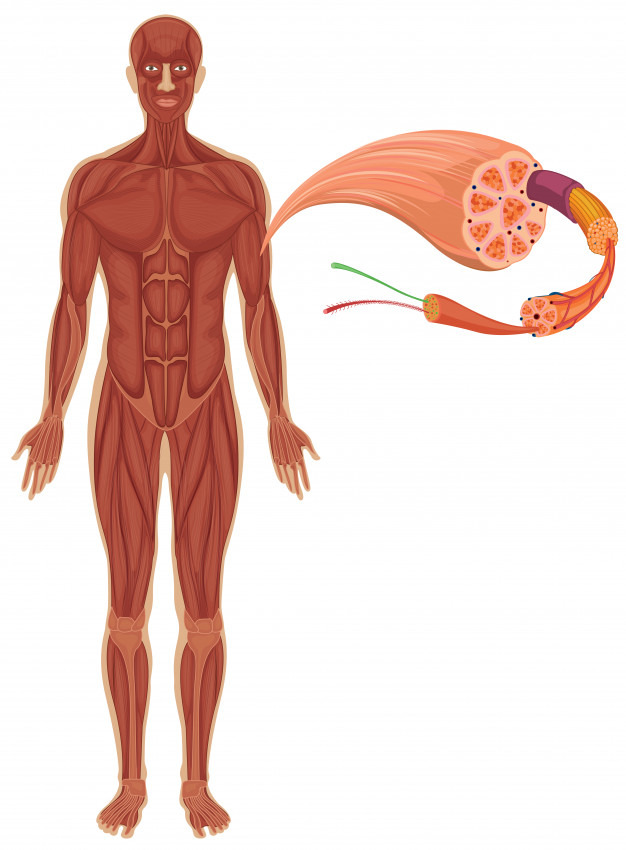
Turning to less controversial life-saving technology advances “Defibrillation”, is alternatively referred to as electrical cardioversion, a medical procedure that uses an electrical current to modify a person’s heartbeat, with the goal of returning the heart to a normal, healthy rhythm. Various conditions and medical events can result in potentially fatal arrhythmias in the lower chambers of the heart, which must be remedied through defibrillation.
While defibrillation is an effective strategy for addressing abnormal heart rhythms, medical professionals will have more success with the technique if they apply it as soon as the arrhythmia develops. Defibrillation technology can manage a variety of abnormal heartbeats, including ventricular tachycardia (defined by a quick heartbeat with no pulse) and ventricular fibrillation (a quivering heart muscle resulting from cardiac arrest).
While defibrillators are often used during medical emergencies, individuals living with potentially fatal heart conditions must carry personal defibrillators with them at all times. These devices range in form from a vest-like, wearable defibrillator to implantable cardioverter defibrillator devices, which are comparable to a watch.
While events requiring defibrillation may be frightening, defibrillation is fairly common in the United States, Every year, about 200,000 hospital patients and 184,000 individuals outside of hospital settings experience cardiac events that require defibrillation.